[This information guide is also available in PDF format to download.]
What are lymph nodes?
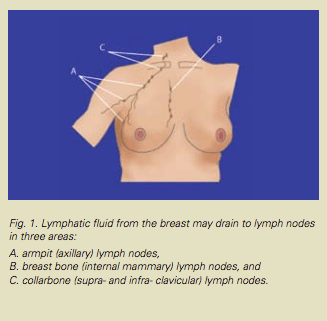
Lymph nodes (also called lymph glands) are part of the body’s immune system. Tiny channels (called lymphatics) carry fluid and debris to the lymph nodes which act as filters. The lymph nodes that filter waste fluid and cells from the breast are mainly located in the armpit (also called the axilla.) These lymph nodes are usually the first ones affected if cancer spreads beyond the breast. Other lymph nodes that can become involved with breast cancer are located near the collarbone and behind the breastbone.
Why do lymph nodes need to be removed?
Treatment for breast cancer usually involves removing some lymph nodes as well as removing the cancer from the breast. Testing the lymph nodes is very important, as it gives you and your doctor information about the breast cancer. This helps to plan further treatment.
Overall, about 70% of women with breast cancer will not have cancer in the lymph glands. The chance of cancer spreading to the lymph nodes is partly determined by the size of the cancer. Smaller breast cancers are less likely to involve the lymph nodes.
How can the lymph nodes be sampled?
In the past, the usual operation for breast cancer was to remove most, if not all of the lymph nodes from the armpit on the same side as the breast cancer. This operation is called axillary clearance or axillary dissection. Axillary clearance is a very effective operation to get information about whether or not the cancer has spread to the lymph nodes. Because all of the lymph nodes are removed, axillary clearance also helps to reduce the chance of the breast cancer coming back in the armpit in the future.
Axillary clearance has some possible side effects. These include:
- stiffness of the shoulder
- numbness of the inner aspect of the upper arm
- seroma (a collection of fluid under the arm in the weeks after surgery)
- lymphoedema (permanent swelling of the arm due to a build-up of fluid in the tissues) — see the ‘Lymphoedema’ Fact Sheet for more information.
What is a sentinel node biopsy?
Sentinel node biopsy is a technique that has evolved over recent years and it is now the usual way to assess the lymph nodes in women with early breast cancer. It aims to avoid some of the side effects of axillary clearance by removing fewer glands. Removing only the sentinel or ‘guardian’ nodes lessens the likelihood of complications and in most cases still provides the necessary information about the cancer. There are still some situations when axillary clearance is needed. If cancer cells are found in the sentinel node then axillary clearance is sometimes recommended.
The sentinel node/s are the lymph nodes that fluid from the breast ‘drains’ to first. Usually there are between one and three sentinel nodes. It is thought that if breast cancer cells were to escape into the lymphatic system, they would travel to the sentinel node/s before moving on to other nodes and the rest of the body.
Sentinel lymph node biopsy is a technique that aims to identify and remove just the sentinel node/s and no others.
Who can have sentinel node biopsy?
Sentinel node biopsy is recommended for patients who have early breast cancer. The breast cancer itself may be removed with wide excision (conserving most of the breast) or with mastectomy (removing the whole breast).
In some cases, sentinel node biopsy is done in conjunction with an axillary clearance.
How is sentinel node biopsy performed?
The sentinel node is identified, or ‘mapped’ using a combination of techniques. These are:
-
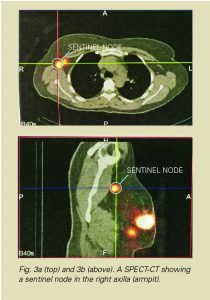
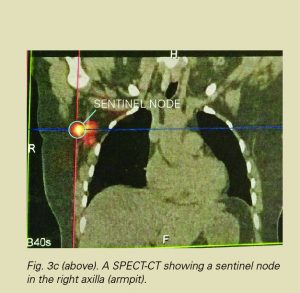
a nuclear medicine test called lymphoscintigraphy (lymphatic mapping) performed before the operation
-
a scan using a hand-held probe performed by the surgeon during surgery
-
a blue dye test, also performed by the surgeon as part of the operation.
These techniques produce a ‘road map’ to help the surgeon find the sentinel node for removal during the operation.
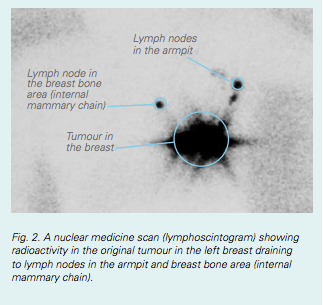
Lymphatic mapping is performed the day before, or a few hours before surgery. It is usually performed in a nuclear medicine or X-ray department. A small amount of radioactive material is injected around the cancer or under the nipple. The radioactive tracer travels from the cancer site to the sentinel node, along the same lymphatic channels that cancer cells could travel. This can take a few minutes or a couple of hours. A series of scans is taken to show where the sentinel node is located.
The injection of tracer makes the sentinel node radioactive so it can be found by the surgeon with the use of a gamma probe (a type of hand-held Geiger counter) during the operation (Fig. 4). The dose of radiation is very small and will cause you no harm.
The blue dye test is sometimes performed at the beginning of the operation. When you are asleep, a small amount of blue dye is injected around the nipple or the cancer. The dye quickly moves into the lymphatic channels and turns the sentinel node blue, again helping the surgeon to locate the sentinel node.

Fig. 4. The sentinel node gamma probe used by the surgeon to detect radioactivity in the sentinel node during the operation.
This combination of blue dye and radioactive material allows a sentinel lymph node to be identified in over 98% of cases.
Depending on the situation, your surgeon may choose to use only blue dye or only lymphoscintigraphy rather than the combination.
Once the sentinel node is found, it is removed and sent for examination by a pathologist. The pathologist, knowing this to be an important node, can perform special tests to identify even the smallest cancer deposits if they are present.
It is important to understand that a lymph node that is successfully ‘mapped’ (i.e., one that shows up on the nuclear medicine or blue dye tests) does not necessarily contain cancer cells. Rather, it is the first lymph node likely to be affected if cancer cells have escaped into the lymphatic system and the one that is examined most thoroughly by the pathologist.
What are the advantages of sentinel node biopsy?
Most women who have breast conserving surgery and sentinel node biopsy have a shorter hospital stay, a smaller scar and a quicker recovery time than women who have all the lymph nodes removed from under their arm (axillary clearance).
Sentinel node biopsy removes fewer lymph nodes than the standard operation of axillary clearance. This lowers the risk of developing lymphoedema, pain and numbness.
What are the possible side effects of sentinel node biopsy?
- A small amount radioactive tracer is used for the lymhoscintigraphy scan.
- The blue dye will turn your urine a blue-green colour for about 24 hours.
- The skin over your breast will also be stained blue for a couple of weeks.
- Mild allergic reactions to blue dye occur in 1-2% of patients.
- Severe allergic reactions to the blue dye are also possible but are extremely rare.
- There may be wounds in the breastbone area as well as the armpit and on the breast.
- Lymphoedema is still possible after sentinel node biopsy but the risk is much lower than it is following full axillary lymph node clearance.
- A false negative result is possible.
What is a false-negative result?
A false-negative result occurs when the lymph node removed as the sentinel (first draining) node does not contain cancer cells, while another lymph node that does contain cancer cells is left behind in the armpit. The rate of false-negative results varies between different breast cancer treatment centres. The chance of a false-negative result ranges between 1% for tumours under 2cm and 3 to 4% or larger tumours.
What if the sentinel node biopsy is ‘positive?’
If the pathologist sees cancer cells in a sentinel node, the biopsy is said to be ‘positive’. If this happens your surgeon might recommend that you have further surgery to remove all of the glands under your arm (full axillary clearance) or have radiotherapy to the glands. In other cases, no further treatment will be needed.
If the sentinel node biopsy is negative (i.e., no cancer cells are seen in the sentinel node), no further treatment to the armpit is required.
When is sentinel node biopsy not recommended?
Some patients with breast cancer are still best treated with complete axillary clearance rather than with sentinel node biopsy. Axillary clearance is usually recommended when the cancer is found in the lymph glands on imaging and biopsy before surgery.
In some of these cases, sentinel node biopsy is performed at the time of full axillary clearance. This is to ensure that if the cancer ‘drains’ to lymph nodes near the collarbone and breast bone areas, these may be sampled.
Useful contacts/websites
| Cancer Australia | canceraustralia.gov.au |
| Cancer Council | cancer.org.au |
| Cancer Council Helpline | 13 11 20 |
| Breast Cancer Network Australia (BCNA) | 1800 500 258 bcna.org.au |
Version 5 – WSP 220 March 2024
© Westmead Breast Cancer Institute
[This information guide is also available in PDF format to download.]
