[This information guide is also available in PDF for download.]
What is breast reconstruction?
Breast reconstruction is a surgical procedure that creates a shape on the chest wall following a mastectomy. Occasionally, it can also be used to improve breast symmetry after a lumpectomy.
Breast reconstruction is an option for most women who have a mastectomy. There are several different techniques that can be used. For some women, one type of reconstruction may be more suitable than another. For others, it will be a matter of personal preference. Factors such as body shape and pre-existing medical conditions can influence the type of breast reconstruction recommended. The stage of your cancer and the need for chemotherapy or radiotherapy are also important factors to consider.
Breast reconstruction can be immediate (performed at the same time as mastectomy) or delayed (performed at a later time). There may be things about your cancer or treatment that make your specialists recommend a delayed reconstruction, but for most women the decision between immediate or delayed reconstruction is a matter of choice and availability of surgical facilities.
If you are considering breast reconstruction, it is a good idea to discuss it with your breast surgeon before your cancer operation. There is no need to feel pressured to make a decision if you are unsure. Many women choose to wait until after their initial breast surgery to decide about reconstruction.
Breast reconstruction is not for everyone, and many women choose to wear an artificial breast form (external prosthesis) in their bra rather than have surgical reconstruction.
How is a breast reconstructed?
There are several different surgical techniques that can be used to create a breast shape on the chest (and to match it to the opposite breast). These include:
-
Breast implant reconstruction (insertion of a silicone gel implant, or insertion of a tissue expander that is replaced later with a permanent silicone gel breast implant)
-
Tissue flap reconstruction (moving tissue from the back, tummy or thigh) to the chest area
-
Reconstruction of the nipple (which usually happens at a later stage, typically 3 to 12 months after the implant or tissue flap reconstruction)
-
Surgery to the unaffected breast so that it matches the reconstructed side better (“symmetrising” surgery).
A woman undergoing breast reconstruction may choose to have one or more than one of these procedures to achieve the best possible result for her.
Breast implant reconstruction
Breast reconstruction using an implant can be performed
-
as a single operation (when a permanent implant is inserted immediately after the mastectomy) or
-
as a two-stage operation (when a tissue expander is inserted after the mastectomy and it is exchanged for a permanent implant at a later operation).
The most suitable option for you will depend on your current breast size, desired breast size, body shape and cancer-related factors. Your surgeon will be able to discuss this with you.
‘Direct- to- implant’ reconstruction
In most cases, the breast skin (and sometimes the nipple) can be preserved at the time of mastectomy. This means that the implant may be able to be inserted directly, without using a tissue expander first. This procedure is not suitable for every case but it may be possible if the cancer is away from the nipple and your breast is a suitable size and shape. Sometimes the implant can be inserted directly even if the nipple is not preserved.
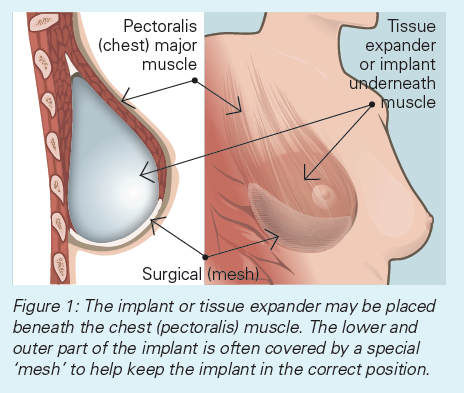
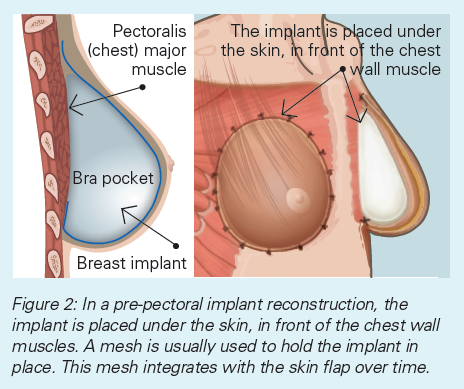
The implant is placed either beneath the chest (pectoralis) muscle, or in front of the chest muscle. Your surgeon will discuss this with you. The lower and outer part of the implant is often covered by a specially manufactured ‘mesh’, which helps keep the implant in the correct position. (Figure 1). If the implant is placed in front of the muscle, the ‘mesh’ covers the whole implant (Figure 2). Sometimes breast skin can be used instead of mesh.
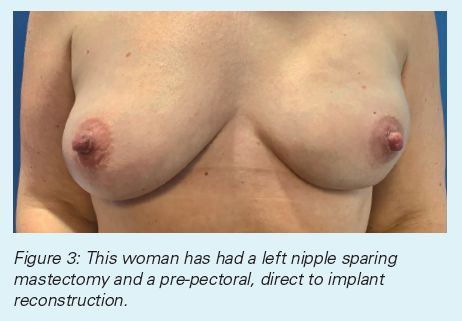
The majority of ‘direct-to-implant’ operations are complex surgical procedures and therefore have a slightly higher complication rate, but these are infrequent. It is important that you have a detailed consultation with your surgeon to make sure that this is the right option for you and to discuss the possible risks. The operation must be carefully planned and this will reduce the risk of problems.
Tissue expander reconstruction
A tissue expander is used when skin and/or muscle need to be stretched to make enough space for an implant, or to avoid tension on the skin flaps after the mastectomy.
A tissue expander is a silicone balloon that can be filled with saline (salt water). It is a temporary implant that is used to gradually stretch the skin and chest (pectoralis) muscle. It is put in under the skin and muscle and it is gradually inflated over a few months by adding fluid through an injection port in the balloon. This ‘inflation’ (or ‘expansion’) procedure is done in the clinic or private rooms as an outpatient procedure.
When the tissue expander reaches the right size, it is removed (usually as a day surgery or overnight procedure) and a permanent silicone gel implant (prosthesis) is put in its place. The permanent prosthesis is softer and more comfortable than the tissue expander and it comes in a range of shapes and sizes to better match the opposite breast and looks more natural.
Sometimes tissue expansion is combined with some form of mesh to help create a more natural looking result.
If you are having radiotherapy with a tissue expander in place, the expander will normally be fully inflated before the radiation treatment starts. If you are having chemotherapy and/or radiotherapy, the surgical procedure to exchange the tissue expander for a permanent prosthesis is usually delayed. Sometimes your surgeon may opt to exchange the tissue expander to the permanent gel implant prior to your radiotherapy.
Whether you have a one-stage (‘direct-to-implant’) or a two-stage (tissue expander) implant reconstruction, you may benefit from fat grafting at a later date to smooth out the skin surface. This is a procedure where some of your own fat is taken from your abdomen or thigh and injected around the implant.
Advantages
The advantages of an implant-based reconstruction are that:
- the operation is relatively short
-
the recovery time is much quicker than it is with a flap (tissue) reconstruction
-
the only area that needs to heal is the breast/chest area
Disadvantages
-
It is difficult to reconstruct a very large breast with this technique, unless the reconstruction is combined with a procedure to reduce the size of the opposite breast.
-
An implant will not ‘droop’ over time the way a normal breast will, so over time the difference between the reconstructed breast and the normal breast may become more obvious.
-
It may be possible to feel the edges of the implant if the skin flaps are thin (so called rippling)
-
An infection may potentially occur which usually can be treated with antibiotics and/or specialised dressings. It is important that you contact your surgeon immediately if you develop any signs of infection, such as redness.
-
In some cases, implants need to be replaced over time, due to the development of ‘capsular contracture’, a condition in which the implant becomes hard and may lose its shape. The risk of this happening is significantly higher after radiotherapy. It is also possible that the implant will need to be replaced in the future as it ages.
-
Some women may feel the implant position has shifted over time.
-
Although it may be possible to use tissue expander/implant reconstruction after radiotherapy, the result may not be as good as in women who have not been treated with radiotherapy. This is because radiation to the chest wall can make the skin and muscle tighter and therefore more difficult to stretch. In this circumstance, your surgeon may recommend a tissue or flap reconstruction (see below).
Tissue flap reconstruction
A flap reconstruction uses your own body tissue. A flap of fat, skin and/or muscle is taken from the abdomen or back, and the tissue is moved to the chest to re-create a breast shape. This type of breast reconstruction is more complicated than an implant procedure, but the final result may look more natural. Sometimes your surgeon may recommend a combination of flap and implant construction.
Flap reconstruction is not suitable for everyone. For example, women who are very thin may not have enough tissue on their abdomen to create a breast shape of the right size. Women who have had previous major abdominal surgery may also be unsuitable for this type of reconstruction. Flap reconstruction requires healthy blood vessels, women who have diabetes, connective tissue disease, vascular disease, or women who smoke, may need to consider other options.
Possible complications of flap surgery include weakness at the site where the muscle was taken from, and (rarely) there can be problems with the blood supply to the flap, and the flap tissue may not survive.
Advantages
-
A flap reconstruction can give a very natural looking reconstruction
-
The reconstruction will change with the rest of your body. If you lose or gain weight the reconstructed breast will change too.
-
It is a good option for delayed reconstruction after radiotherapy.
Disadvantages
-
A flap reconstruction is a long operation and usually takes at least four hours to perform.
-
The recovery time is much longer than it is with an expander/implant reconstruction, as there is an abdominal or back wound as well as a breast wound to heal.
-
A flap reconstruction may shrink if radiotherapy is given after reconstruction.
1. Flap from the lower abdomen – Transverse rectus abdominis muscle (TRAM) flap, or deep inferior epigastric perforator (DIEP) flap
The tissue from the lower abdomen is moved to the chest area. The blood supply may be disconnected and reconnected to arteries and veins in the chest with microsurgery (free flap) or it may bring its own blood supply (pedicle flap). These flaps result in a ’tummy tuck’ effect as well as a breast reconstruction.
2. Flap from the back – Latissimus dorsi (LD) flap
The tissue from the back is tunnelled under the skin to the front of the chest, bringing its own blood supply. Sometimes a breast implant or tissue expander is put under the flap for extra volume. Other sites that may be considered by some surgeons for use are the thighs or buttocks.
Reconstruction of the nipple and areola
Reconstruction of the nipple and areola is optional and is usually done as a separate procedure a later stage (when the swelling from the original operation has settled). There are a number of different surgical techniques that can be used to reconstruct the nipple and areola.
Expert tattooing can also give a very realistic appearance. Another option is the use of a self-adhesive silicone nipple.
Surgery to the other breast
Sometimes your surgeon may recommend surgery for your other breast to achieve better symmetry. A breast reduction, ‘lift’ or enlargement may be discussed. This surgery can be done at the same time as the reconstruction or as a separate procedure after cancer treatment is finished. See figure 2.
What will my reconstructed breast look like?
It is important to understand what breast reconstruction can realistically achieve. A reconstruction cannot give you a new, normally functioning breast. The aim is to provide a contour or shape to your body so that you will be able to wear most types of clothing, including swimwear.
What are the benefits of breast reconstruction?
Many women feel that breast reconstruction helps them deal with the emotions associated with losing their breast. Some women feel more self-confident and feminine after they have had a reconstruction.
After a breast reconstruction, there is no need to wear an external prosthesis in a bra, which means there are more options for the clothes you can wear. Many women say they feel more ‘normal’ after a reconstruction and more comfortable in the clothing they wear.
How does breast reconstruction affect my breast cancer treatment and follow-up?
Reconstruction does not usually interfere with breast cancer treatments such as radiotherapy, chemotherapy or hormone-blocking therapy. It is important that your doctors coordinate the different parts of your treatment so that the reconstruction does not delay important cancer treatment. There may be some situations when your cancer specialists recommend delayed rather than immediate reconstruction to make sure that cancer treatment is not delayed.
When breast reconstruction is combined with radiotherapy, there are some special considerations. When radiotherapy is given after a reconstruction, there may be hardening around an implant or shrinkage of a flap. When breast reconstruction is done after radiotherapy, there may be scarring in the chest muscles making an implant reconstruction difficult or impossible and a flap reconstruction may be the only option. Your surgeon can discuss all of these things with you and help to plan the best sequence for you.
Breast reconstruction does not interfere with cancer follow-up care. Recurrence of cancer after a mastectomy is a very uncommon situation; however it is not affected by reconstruction, and if your cancer was to recur, it would still be able to be found.
What are the limitations of breast reconstruction?
Breast reconstruction is not able to restore the appearance and shape your breast had before mastectomy. The reconstructed tissue will also not have the same sensitivity.
If breast reconstruction is immediate (done at the same time as mastectomy), the time in hospital and the recovery time is longer than it would be if no reconstruction was done.
Breast reconstruction can have some long-term side effects, such as scar contraction around an implant, or shrinking of a flap. This can be a particular problem after radiation therapy. These changes can make your tissue and skin feel tight and less mobile.
You may go through a period of emotional readjustment as you begin to think of your reconstructed breast as your own. Talking to other women who have had breast reconstruction, or to a counsellor, may help you. Some women find it helpful to communicate with other women who have been through the experience.
What will my recovery be like?
Implant reconstruction
You are likely to feel tired and sore for a few weeks after the first stage of an implant reconstruction (when the tissue expander or implant is inserted). It may be several weeks until you are able to do most everyday activities without pain or discomfort.
Most women are in hospital for one to three days following surgery and a drain (plastic tube that drains fluid from the chest area) is in place for one to two weeks after the operation. You may be discharged from hospital with the drain in; if this happens you will be shown how to look after it or a nurse will visit you at home to help you.
Your surgeon is likely to recommend that you do not do any heavy lifting, repetitive arm movements or high-reaching activities such as vacuuming and hanging out washing for four to six weeks following an implant reconstruction. There may also be limitations on everyday activities like lifting children and carrying shopping bags. You should check with your surgeon about what you are allowed to do following your surgery.
The recovery is much quicker after the second stage of the reconstruction (when the tissue expander is exchanged for a permanent prosthesis). If you have the operation as a single-stage operation (for example nipple-sparing mastectomy and insertion of permanent prosthesis) the recovery is similar to the recovery after the first stage of a tissue expander/implant reconstruction.
Flap reconstruction
The recovery from a flap reconstruction is longer than from an implant procedure, especially if it is an abdominal flap reconstruction because the donor site (the area the flap was taken from) also needs to heal. You are likely to feel tired and sore for several months after flap procedures. Many women find that the abdominal area feels uncomfortable for longer than the breast area does. This discomfort can be controlled with pain medication. Most women are in hospital for around a week after a flap reconstruction. It is likely that you will be discharged from hospital with a drain in place. Sometimes it is necessary to leave a drain in place for two weeks or more. Patients are often required to wear a garment that resemble corset-pants that the patient can purchase or an abdominal binder from the hospital. The patients need to wear these for at least 4 weeks after surgery. This will help to control any fluid build up. Also the patients are often told not to wear a bra for 4 weeks, and thereafter to avoid bras with an underwire.
Your surgeon will usually recommend that you limit your activities in the immediate weeks after a breast reconstruction operation. You should check with your surgeon as to what you are allowed to do following your surgery. The limitations may be in place for longer after a flap reconstruction than an implant reconstruction.
Can I have a reconstruction later?
Many women choose to think about breast reconstruction a little further down the track from their cancer diagnosis. This may be because a surgeon or oncologist recommends delayed instead of immediate reconstruction. Sometimes it is because a woman decides to focus on the cancer treatment and think about reconstruction later. It is never too late for a breast reconstruction. The options depend on the cancer treatment you have had and may change with time. For example, only some types of reconstruction may be possible after radiotherapy.
What will breast reconstruction cost?
Breast reconstruction after surgery for the treatment or prevention of cancer is fully covered by Medicare in the public hospital system. It can also be done through the private health system although this will usually involve some out-of-pocket expenses. Your surgeon can give you more details about this.
What will happen to the reconstructed breast over time?
Most scars from breast cancer surgery will fade and soften over time, so the breast may look and feel more natural as the years go by. Some feeling returns to the skin in the reconstructed area over several years, but it is never the same as it was before the mastectomy.
Sometimes further surgery is recommended in the future. This is usually for minor adjustments to the position or shape of the reconstructed tissue or to improve the scars. Sometimes implants need to be replaced over time and this is difficult to predict.
Who can I talk to about reconstruction?
Your cancer surgeon can discuss your options with you, and some cancer surgeons routinely perform breast reconstruction surgery. In some cases you may be referred to a plastic surgeon for consultation. Your breast care nurse can also talk to you about breast reconstruction.
Where can I find more information?
Breast prostheses and reconstruction – Cancer Council Australia
https://www.cancer.org.au/about-cancer/publications.html
Breast reconstruction – Cancer Australia
https://breast-cancer.canceraustralia.gov.au/treatment/surgery/breast-reconstruction
Breconda (Breast reconstruction decision aid)
https://www.bcna.org.au/resource/breconda
Reclaim Your Curves
https://www.reclaimyourcurves.org.au
Questions to ask your doctor
It is important that you find out as much as possible about breast reconstruction before you make decisions. It is often helpful to make a list of things you would like to know before you see your doctor. The questions below are examples of questions women may ask their surgeon.
About the choices
-
What type of breast reconstruction do you recommend for me?
-
Is there a procedure that would suit my body shape best?
-
Is there a procedure that would suit my lifestyle or job best?
-
What is the most common type of reconstruction?
-
What is a skin-sparing or nipple-sparing procedure?
About the operation
-
How long does the operation take?
-
How long will I be in hospital?
-
Will there be drains?
-
Will I have a lot of pain?
-
Who will do the operation?
-
What are the possible complications of the surgery?
-
Are there any dangers with breast implants?
About the recovery
-
How long will it take to recover?
-
Are there any restrictions to my activities following surgery?
-
When can I drive a car?
-
When can I go back to work?
-
When can I start walking for exercise? Jogging? Going to the gym?
About the costs
-
Which hospital do you recommend for the surgery?
-
Is the operation covered by Medicare?
-
Are there any out-of-pocket expenses?
-
Is there a waiting list?
About other treatments for cancer
-
Do you think I will need radiation treatment or chemotherapy? Should these treatments affect my choice for reconstruction?
-
Will breast reconstruction affect my other cancer treatment?
About the future
-
Will a reconstruction make the cancer more likely to return?
-
Do I need to have a mammogram on the reconstructed tissue?
-
What will my reconstructed breast look like in 10 years? 20 years?
-
If I have an implant reconstruction will the implant need replacement?
Useful Contacts / Websites
| Cancer Australia | canceraustralia.gov.au |
| Cancer Council | cancer.org.au |
| Cancer Council Helpline | 13 11 20 |
| Breast Cancer Network Australia (BCNA) | 1800 500 258 bcna.org.au |
[This information guide is also available in PDF for download.]
Version 5 – WSP 183 September 2024
© Westmead Breast Cancer Institute 2020
